Testosterone Replacement Therapy – Is it time for it?
Typically starting at about the age of 30, a man’s testosterone levels drop by about 10% every decade. Together with that, sex binding hormone globulin (SHBG) levels start to increase, “trapping” much of the circulating testosterone and making it effectively unavailable to exert its expected effects on the body. The resulting difference between the total testosterone and the bound, unavailable is what we call free or “bioavailable” testosterone and, more importantly than the total levels of the hormone, plays a major role in the health, drive, quality of life and performance of an individual.
Every man will experience a decline in free testosterone as age comes, but some men will experience it harder and faster than others. The reason for that may be physical, psychological, environmental or as a result of years of natural-production suppression due to steroid usage when younger. When this happens, these men will go through a variety of negative symptoms that can severely impact their day-to-day life and even expose their health to the long-term risks of low testosterone. Some of these risks are:
- Cardiovascular disease
- Cancer
- Diabetes
- Osteoporosis
- Depression
- Alzheimer’s
- Erectile Dysfunction
- Metabolic Syndrome
The last one, metabolic syndrome, may very well be the most common one, and is linked to an insulin-sensitivity condition, believed to be related to type 2 diabetes. It can be defined as the presence of 3 out of 5 of the following risk factors:
- Abdominal fat: waist circumference above 40 inches in men; 35 inches in women.
- Elevated blood pressure: greater than 140/90 mmHg.
- Decreased HDL “good” cholesterol: less than 45 mg/dL in men; less than 50 mg/dL in women.
- Elevated triglycerides: greater than 150 mg/dL.
- Elevated fasting glucose: greater than 110 mg/dL.
Ok, so at this point we’ve established some of the major risks of low testosterone levels in aging men, but how can you tell if you’re suffering from low testosterone levels? This is usually done via bloodwork, but as the hormone levels naturally fluctuate significantly throughout the day or the week (i.e., if you have been eating and sleeping properly, if your week has been especially stressful or busy), usually at least a few test results under different conditions are required for accurate diagnosis. If one’s testosterone levels are often beneath the physiological levels (male: 300 to 1,000 nanograms per deciliter (ng/dL) or 10 to 35 nanomoles per liter (nmol/L) or female: 15 to 70 ng/dL or 0.5 to 2.4 nmol/L), then that person is a candidate for testosterone replacement therapy. Other than that, while the range is extensive, an individual with low testosterone will experience one or more of the following clinical symptoms:
- Frequent emotional changes
- Diminished sex drive
- Some form of erectile dysfunction (or less rigid erections)
- Decreased morning erections
- Decreased strength and/or muscle mass
- Decreased feeling of well-being
- Reduced mental quickness and sharpness
- Decreased energy, strength and endurance
- Less desire for activity and exercise
- Increased body fat
- Night sweats and trouble sleeping
- Some level of depression and irritability
- Loss of enthusiasm for daily life
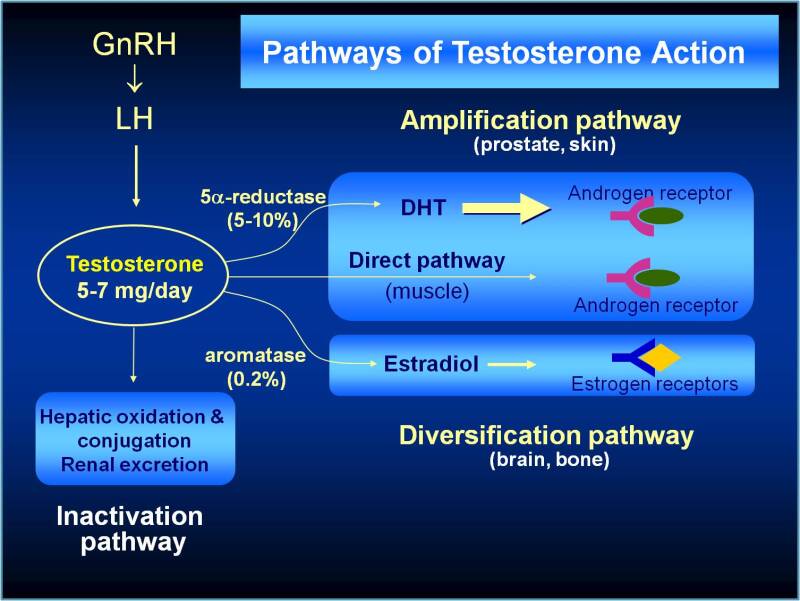
Say you’ve established you need to undergo a TRT program, how do you do it? The best way is of course going to a specialized doctor and following his directions. If you want to do it by yourself, though, a good starting point is trying to replace the 5-7mg/day of testosterone that a healthy adult male typically produces with testosterone injections. To save you the math, accounting for the ester availability, that will be around 100mg of injectable testosterone every 10 days (50 mg of testosterone cypionate or enanthate every 5 days would be better to mitigate ups and downs in seric levels). This will probably be enough to keep you in the physiological levels of testosterone action, but further bloodwork is advised to make sure. More than that and you’re no longer in TRT range, but rather doing a steroid cycle.
Other options include the use of transdermal gels and creams, patches, pellets and implants. To stay within physiological testosterone levels range, you will need to check the concentration and bioavailability of the chosen method in order to work out your dose.
However, it may not be that simple. Some individuals may need to use other medications during their TRT programs. These include:
- Aromatase inhibitors (Anastrozole/Exemestane): AI’s block the conversion of testosterone into estrogen. TRT patients who suffer estrogen elevations above the top of normal range are often given an aromatase inhibitor.
- Selective Estrogen Receptor Modulators (SERMs), (Nolvadex/Tamoxifen): SERMs hinder the action but not the production of estrogen. In TRT contexts, this drug is usually taken to counter the physical manifestations of estrogen-related problems like gynecomastia.
- Human Chorionic Gonadotropin (hCG): even at TRT does, Testosterone supplementation suppresses natural production. Over time, this can lead to testicular atrophy. hCG helps restore and maintain Testosterone production and testicular size by mimicking LH and stimulating the production and release of natural Testosterone.
- 5-Alpha Reductase Inhibitors (Finasteride, Dutasteride/ Propecia, Proscar): These drugs are specific inhibitors of the 5a-reductase, the enzyme responsible for conversion of testosterone to dihydrotestosterone (DHT). In men, DHT has its own pros and cons. DHT is three times more potent than Testosterone, doesn’t aromatize to estrogen, and is associated with high libido. However, it’s also linked to male pattern baldness, acne, and prostate cancer.
As you can imagine, it gets a lot more complex when you add these other drugs to the mix. If you’re going down that route, I strongly advise you to seek professional help.
Overall, the health benefits to be gained overwhelmingly seem to support Testosterone replacement when you consider the beneficial effects to energy levels, metabolism, muscle mass/functionality, and even blood chemistry and cardiac health, if done correctly.