Insulin sensivity and protocols
Pathophysiological alterations in glucose tolerance
- On average, a healthy adult human has about 90mg / dL of glucose in an 8-hour fasting state; the level of normality ranges from 70 to 110mg / dL, qualifying any measurement between 110 and 125mg / dL as pre-diabetes and from 126mg / dL onwards, as diabetes.
- Insulin is secreted by the Pancreas in response to the alterations it perceives in blood glucose levels, so although glucose levels remain more or less within a few ranges throughout the day, Insulin levels fluctuate a lot. depending on the meals we make.
- Insulin has a receptor on the cell membrane in tissues such as the muscle where, once it binds to it, a cascade of molecular signaling begins (whose last step is the phosphorylation of Akt) that aims to induce the migration of glucose transporters (GLUT) from the cytoplasm to the cell membrane to take up glucose.
How to know if you have low insulin sensivity
To evaluate your glucose sensitivity status, one of the best and least invasive ways is simply to do a HOMA-IR (which is nothing more than a value that is derived based on your insulin level and fasting glucose), and if possible, combine it with a cortisol measurement to rule out the possibility of a false positive due to a dawn phenomenon due to the stress that may be generating the analysis (although even in the worst case, HOMA-IR should be within normal parameters).
Intracellular signaling cascade for glucose uptake.
The first four steps of the process consist of the union of insulin to its receptor and the entire intracellular signaling cascade that occurs, migrating GLUT receptors towards the membrane surface to capture glucose.A phosphate group is added (phosphorylation), imagine it as a stack P, which once it binds to the protein, it turns it on. The next steps are the formation of Malonil-CoA to carry out de novo lipogenesis, this in turn inhibits CPT-1 (Carnitine Palmitoyltransferase, an enzyme that transports fatty acids to the mitochondria using carnitine as a “vehicle” transport), causing less fatty acids to enter the mitochondria to be oxidized and, therefore, increasing the amount of fatty acids present in the cell.
Glucagon and its role
The pancreas in addition to having beta cells, which secrete insulin, also have alpha cells that secrete glucagon.
Glucagon is a hormone that has several functions but all with the same purpose: to stimulate the production and release of glucose and to inhibit glycolysis (burning of glucose).
Summarizing:
- It stimulates the amount of amino acids taken up by the liver to produce glucose (neoglycogenesis).
- Stimulates the release of catecholamines.
- Stimulates the release of liver glycogen in the form of glucose
- Stimulation of the creation of ketones.
The curious thing about Glucagon is that its release is not regulated based on blood glucose, but based on the release of insulin by the beta cells of the pancreas, so it can be said that its secretion is based on paracrine regulation. ; So if they perceive that the pancreas is secreting insulin, it can be said that they intuit that glucose levels are high and therefore, they do not release anything, if on the contrary, they see that the beta cells are not secreting just insulin, they intuit that glucose is low and they get to work.
Type 2 diabetes (caused by being resistant to insulin).
It has two main causes:
Insulin resistance
- It is understood as such the phenomenon in which when insulin binds to its receptor on the surface of the cell membrane, the intensity with which the intracellular signaling cascades are produced are weaker, therefore, there is not as much displacement of GLUT receptors per unit of insulin, do you remember that the transport of fats to the mitochondria was inhibited and the amount of fatty acids present in the cell was increased? that’s what produces insulin resistance.
- Therefore, taking into account the normal physiology of the human being, the person responsible for insulin resistance is a caloric surplus, since insulin resistance is a cellular defense mechanism against excessive consumption of calories, since By preventing glucose from entering the cell, it increases the oxidation of fatty acids, reducing lipotoxicity due to the accumulation of lipids and with it, lipoapoptosis, in fact, as an interesting fact, VERY VERY obese subjects are VERY sensitive to insulin due to the positive correlation between adipose tissue and insulin sensitivity (Unger & Scherer, 2010).
Pancreatic cell dysfunction
- The accumulation of fats inside the cell produces what is called ectopic lipid deposition (in addition to the release of different undesirable adipokines), which is nothing more than the accumulation of fat outside the subcutaneous adipose tissue (visceral fat), this fat it produces the aforementioned lipotoxicity and with it, lipoapoptosis.
- When it occurs in the pancreas, in the beta cells, this causes them to no longer function properly and therefore, they do not respond adequately to changes in blood glucose. The same is true of the alpha cells of the pancreas; Due to lipotoxicity, they become resistant to insulin, which is why they are constantly secreting glucagon (hyperglucagonemia), which is why diabetic subjects, even when fasting, have such high glucose levels, as well as using strips of Ketone bodies in type 1 diabetes to assess the risk and intensity of ketoacidosis.
This is the reason why drugs like Berberine or Metformin work so well, because they inhibit hepatic neoglycogenesis.
How to improve insulin sensitivity.
We have two mechanisms that will be useful for our objectives.
Via AMPK
- Most of the Fitness sector antagonizes the AMPK and mTOR pathways but AMPK and mTOR are not necessarily antagonistic, after a workout the expression of mTOR is at its peak, which occurs in the presence of a higher expression of AMPK.
- With the activation of mTOR by the abundance of proteins, with leucine standing out, you should not see increases in AMPK at the same time. AMPK is “activated” when a cell detects a lack of nutrients in the form of an increase in ADP and a decrease in ATP levels. The reaction, that is, increased expression of AMPK will have subsequent effects on glucose uptake and fatty acid oxidation, both of which contribute to the restoration of normal ATP levels in the cell.
- Both AMPK and mTOR act in a very localized way. Exercise-induced glucose uptake is therefore muscle-specific, which should be obvious, as exercise will raise ADP levela. Supplements that mimic this effect, on the other hand, act systemically.
- Therefore, agents such as alpha lipoic acid or Metformin (and Berberine) with a systemic effect will increase glucose absorption in both muscle and adipose tissue (as can be seen in the clinical trials of Moini, 2002). After a workout and at other times, where glucose uptake is already high and, more importantly, muscle specific, it is not necessarily the best idea to try to “intensify” the effects by using certain types of supplements.
Via PPAR-GAMMA
Looking at the effects of PPARs, it can be extrapolated that if you block PPAR-gamma, you can inhibit the uptake of energy by adipose tissue.
- The Fedor & Co. results show that these effects can be ameliorated if the suppressant PPAR-gamma (ie, conjugated linoleic acid) is combined with a supplement that exerts the opposite effects on the liver; DHA from fish oil.
- Whether the PPAR-gamma blocking is good or bad obviously depends on the scenario we are talking about. For an individual with little fat, who exercises regularly and wants to reduce the accumulation of body fat as much as possible in an environment of a hypercaloric diet, it is possibly a good thing, since thanks to physical exercise and controlling his percentage of body fat, it is difficult there is no accumulation of fat at the liver and visceral level in general.
- However, in the case of obese and sedentary individuals, especially in the context of a hypercaloric diet, these would be completely contraindicated.
- As paradoxical as it may seem, the antidiabetic effects of thiazolidinediones, which are activators of PPAR-gamma, exert their effects at the expense of increased body fat storage. The latter can be quite pronounced (Bray and Co pre-diabetic clinical trials).
Stacks to improve insulin resistance in bodybuilders.
Normally insulin resistance will have been caused by the use of HGH and insulin, as we have seen previously, the most useful thing will be to reduce liver inflammation.
- Berberine (I prefer this option over Metformin since they have almost the same potency and Berberine lacks the harmful effects on the stomach typical of Metformin, I recommend the HCL version): it exerts its effects via AMPK and PPAR-G, consume 1000 to 1500mg divided into two daily intakes.
- ALA (choosing the R-Ala version): exerts its effects through the AMPK pathway, consume 500 to 1500mg.
- Chlorogenic Acid: exerts its effects through the AMPK route, consume 500 to 1000mg divided into 2 or 3 doses.
- Taurine: exerts its effects since it is a powerful anti-inflammatory and anti-oxidant, consume 3 to 6 grams daily divided into 3 doses.
With these supplements we will exert the effects described on the AMPK and PPAR-G pathways combined with an anti-inflammatory effect on the liver.
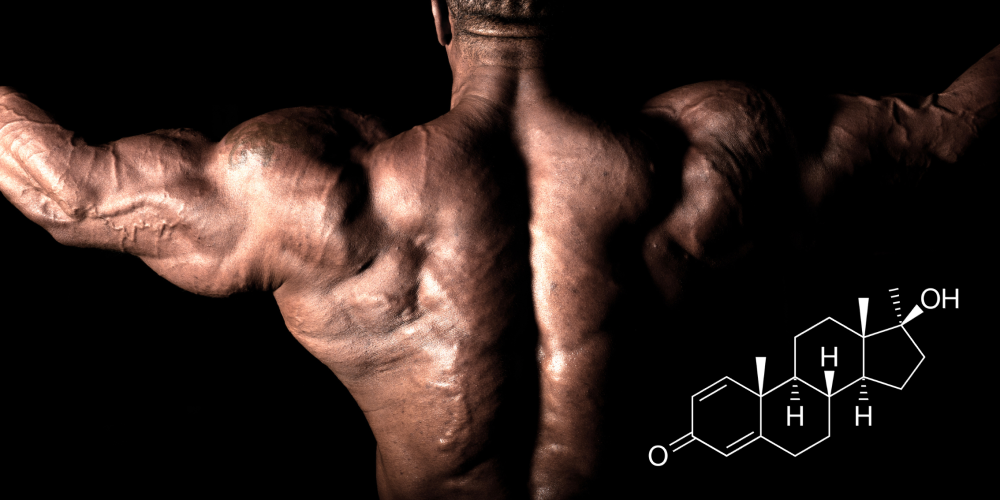
Exogenous insulin
- Increases the rate of glucose transport to the cell membrane.
- Increases the speed of protein synthesis in muscle, adipose tissue, liver and other tissues.
- Stimulates the synthesis of fatty acids and triacylglycerol in tissues.
- Increases the absorption of triglycerides from the blood into adipose tissue and muscle tissue.
- Increases the speed of glycogen synthesis.
- Increases the speed of transport of some amino acids to the tissues.
- Decreases the rate of fatty acid oxidation in muscle and liver.
- Decreases the rate of protein breakdown in muscle.
Ways to inject insulin
- SubQ route (It is the simplest): I recommend rotating the injection site to avoid lipodystrophy, if the injection site is heated, it is absorbed up to 50% faster than indicated by the manufacturer.
- Via IM: Its effect is fasteror what the one with the via SubQ but with the advantage that it does not generate lipodystrophy.
- IV route: It has a half-life of 12 minutes and in about 80 minutes there is no trace of insulin or its activity, so the Cmax is 3 times higher than with any other route of administration, it is reasonably dangerous.
General protocols with exogenous insulin
For any of these protocols I ALWAYS recommend the use of ultra-rapid insulin.
- Protocol 1: inject 30 minutes before training to facilitate the transport of nutrients and take advantage of the hyperemia (increased blood in an organ or in a part of it) produced by the training.
Dose: 1IU for every 10kg (22lbs) of body weight, consume 10 to 5 grams dand carbohydrates per IU of insulin, combine with a low-fat protein isolate.
- Option 2: 5-10 minutes before meals, avoid consuming fat during these meals.
Dose: 1UI for every 5-10gr of carbohydrates consumed at each meal.
- Option 3 (relatively dangerous): 10 minutes pre-cardio on an empty stomach intravenously to force to which the Somogy phenomenon is given by which an increase in the levels of GH, glucagon and catecholamines (among others) for promote the release of fatty acids and their subsequent burning.
Dose: 1IU.